Definitions: Billing Types
Add and customize billing types available for patients and insurance plans.
In the Main Menu, click Setup, Definitions, Billing Types.
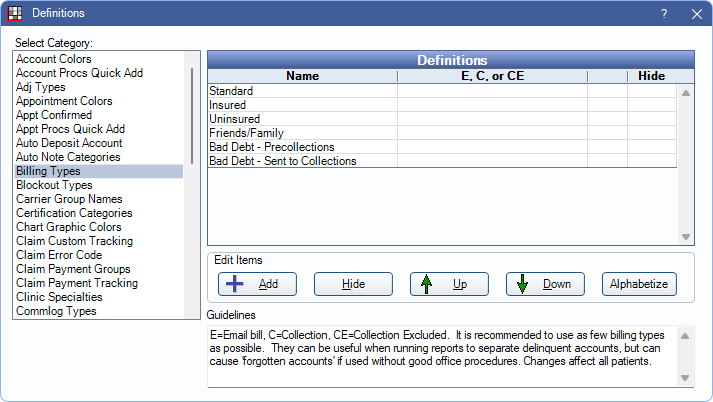
Billing Type options are available in the Edit Patient Information and Edit Insurance Plan windows. Set the default Billing Type in Practice Setup.
Create Billing Types to indicate how a patient is to be billed (e.g., email statements, send to collections, etc.).
Double-click an existing item or click Add to create a new item. The Edit Definition window opens.
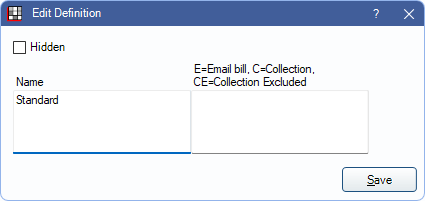
Name: Enter the Billing Type name.
Set the behavior of the Billing Type.
- Enter E to email statements to patients assigned this Billing Type. Statements are emailed when sent from the Billing List.
- Enter C for use with patient accounts sent to TSI for collections. Note: If multiple C Billing Types are created, only guarantors assigned first in the list are included in the TSI Sent Accounts tab. Using a single C Billing Type is recommended, and it should not be added to a preexisting Billing Type already in use.
- Enter CE for use with patients excluded from TSI collections. Note: If multiple CE billing types have been created, only guarantors assigned first in the list are included in the TSI Excluded Accounts tab. Using a single CE Billing Type is recommended, and it should not be added to a preexisting Billing Type already in use.
- Leave blank for standard billing. From the Billing List, statements are printed to be mailed or sent electronically if Electronic Billing is set up in Billing Defaults.
Hidden: Billing Types may be hidden. However, if in use, hidden Billing Types may be visible throughout various areas of the program. If Adding new primary insurance plan to patient sets billing type is enabled in Preferences, and an insurance plan is assigned a hidden Billing Type, adding the insurance plan to a new patient will still change the patient to the hidden Billing Type.
Click Save to exit the window and keep changes.

