Insurance Refunds
If insurance overpays on a Claim, they may either request a refund check or allocate the overpayment to another claim.
Refund via check
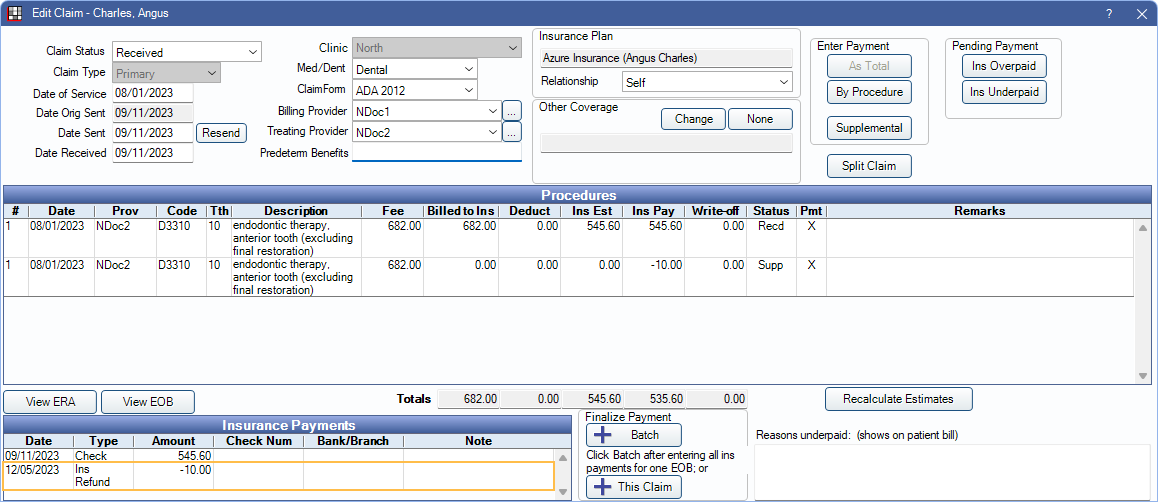
- In the Account Module, double-click on the claim.
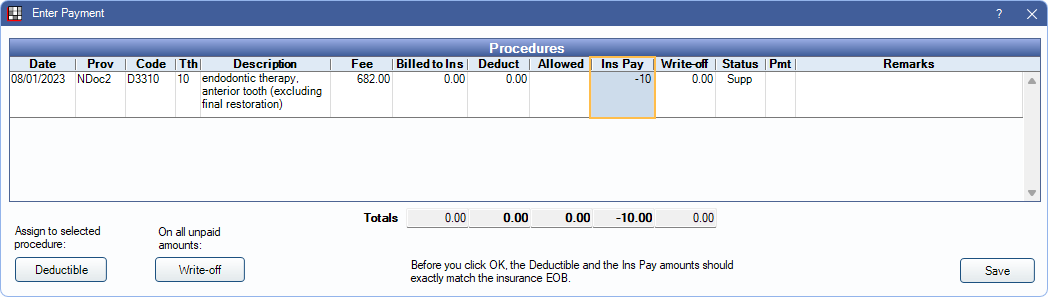
- Highlight the procedure to be refunded
- Click Supplemental at the upper right.
- Enter the refund amount as a negative amount for Ins Pay (e.g. -10), then click Save.
- In the Claim, click This Claim Only.
- Enter any needed check information and enter the payment amount as a negative (e.g. -10).
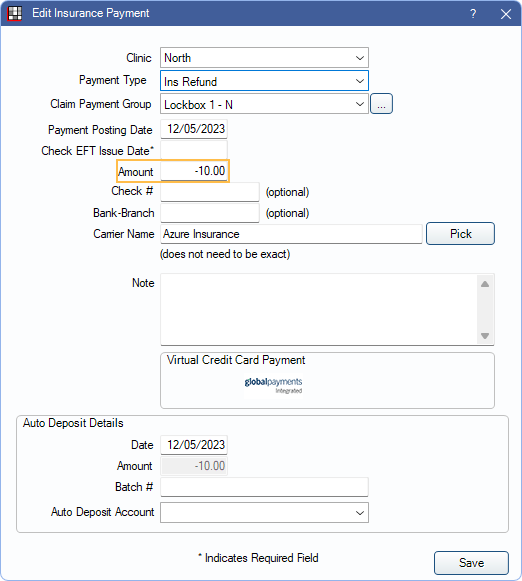
- Complete the rest of the payment as normal. See Finalize Insurance Payment.Note:
- Offices may wish to create a new Insurance Payment Type for Insurance Refund checks to avoid incorrect totals if using Deposit Slips.
- If a payment is being refunded due to eligibilty, additional supplemental payments may be needed to adjust off write-offs as well.
This corrects the patient account balance making the patient responsible for the previous overpayment. If the patient is not responsible for the balance, enter a subtraction Adjustment to remove the amount from the account balance.
Allocate to a different claim
There are times when instead of having an office send a refund check back to the carrier, the carrier deducts the overpayment from another claim payment. This may be on a future claim from the same patient or an entirely different patient, but the process is still the same.
A negative supplemental payment is entered into the overpaid claim (as described above), but instead of finalizing a negative payment, the payment is batched together with the positive payment.
- Double-click the claim that was overpaid and needs to be refunded.
- Follow steps 1-4 from Refund via Check above to enter the overpayment as a negative supplemental payment.
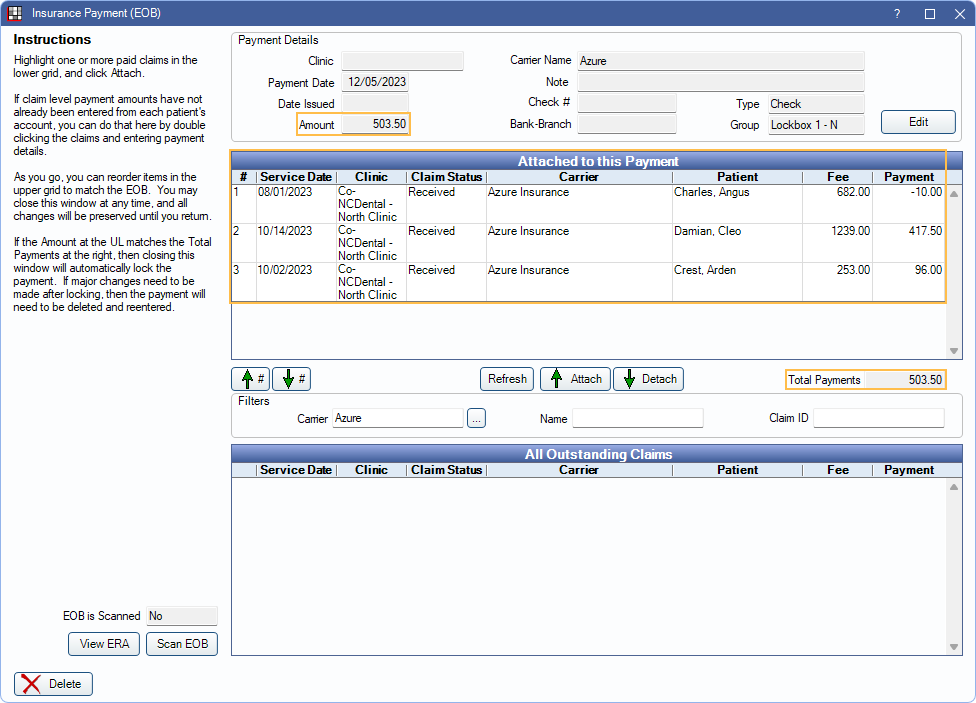
- Create a Batch Insurance check from the Manage Module using the Batch Ins button.
- Attach the refunded claim to the bulk payment.
- Receive all other claims on the EOB and attach them to the payment. (See:Batch Insurance Payment for detailed instructions.)
- Once all claims on the EOB are received, the total payments of the attached claims should match the amount of the payment. The payment is already finalized.