Electronic Eligibility and Benefits
Eligibility requests retrieve benefit information from a Clearinghouse.
In the Insurance Plan window, in the middle, click Request.
Electronic eligibility and benefit information allows staff to electronically verify a patient's insurance eligibility and benefits in real time (e.g., percentages, deductibles, maximums, limitations, and history). Non-subscriber benefits that are not identified as family coverage are inserted as patient override benefits.
Electronic Eligibility checks can be run as a batch by creating a Scheduled Process.
The following third-parties are known to offer eligibility services:
- ClaimConnect (DentalXChange).
- Electronic Dental Services (EDS)
- Trojan
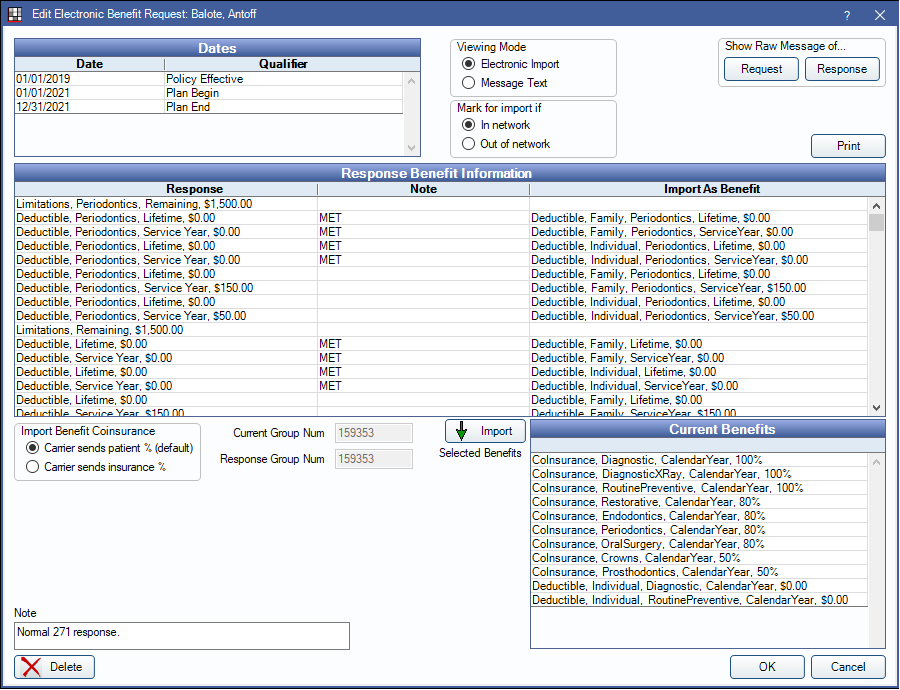
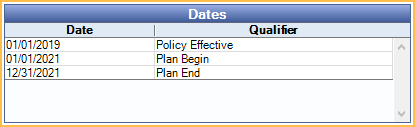
Dates
The Dates grid shows information on eligibility and active service dates.
Miscellaneous Options

Viewing Mode: Select how to view the response message. Options are Electronic Import or Message Text.
Mark for import if: Select whether benefits for In network or Out of network should be imported. Dependent on the practice's disposition with the carrier.
Show Raw Message of...:
- Request: Click to display raw version of the benefit request message sent to the clearinghouse.
- Response: Click to view the raw response message sent by the clearinghouse. See below.

Print: If there are HTML responses, view and print the HTML. Otherwise, the main grid is printed.
Response Benefit Information
This grid displays benefit details received from clearinghouse.
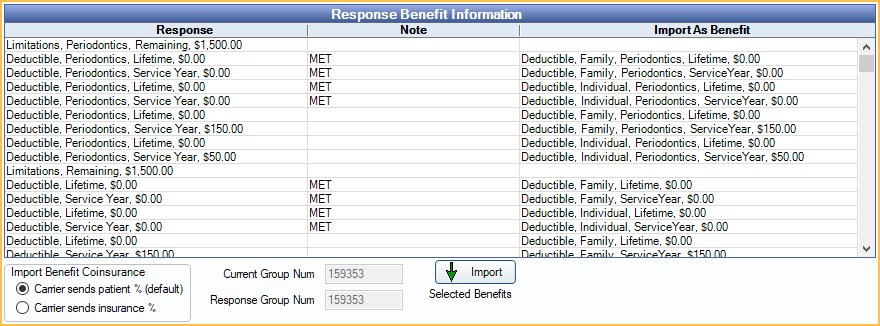
Columns:
- Response: Includes both out-of-network and in-network benefits. Use care in selecting which to import.
- Note: Notes about the benefit.
- Import As Benefit: Displays how the benefit will import into Open Dental.
Import Benefit Coinsurance:
- Carrier sends patient %: Select if benefit response describes patient responsibility. This is the default.
- Carrier sends insurance %: Select if benefit response describes insurance portion.
Current Group Num: The entered group number on the selected patient. A red warning displays if this does not match the group number reported by the carrier below.
Response Group Num: The group number returned by the carrier.
Import: Highlight benefit rows from the grid, then click to import benefits to the patient's plan. Prior to importing, review the highlighted benefit rows and Current Benefits grid (below) to ensure duplicate benefits are not imported.
Double-click a row to open the Raw Benefit Info.

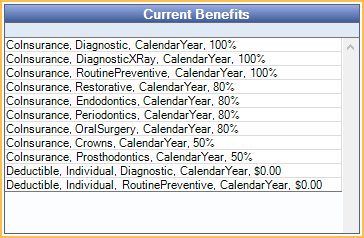
Current Benefits
This grid lists current benefits entered for the selected patient's insurance plan.
Note
Automated text is generated depending on the response. Edit the note as needed.
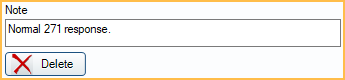
Delete: Delete the response.
Setup
- Register with the vendor. If a clearinghouse, make sure Real Time Eligibility or real time services are enabled.
- Enable the vendor in Open Dental.
- If a clearinghouse, set the clearinghouse as the default clearinghouse for Eligibility:
- Open the Clearinghouses list.
- Highlight the clearinghouse from the list.
- Click Eligibility.
- If clearinghouse details have not been entered previously, double-click the clearinghouse to enter any details.
- If Trojan, enable the bridge, then click Trojan on the Edit Insurance Plan window.
- If a clearinghouse, set the clearinghouse as the default clearinghouse for Eligibility:
- Verify that each carrier's electronic ID is entered accurately in Open Dental (Insurance Plan or Carriers). To determine a carrier's electronic ID, check with the clearinghouse.
View Request History
On the Edit Insurance Plan window, click History. All requests and responses are stored for future reference. Double-click a response to view details.


