Canada Eligibility
For carriers that accept electronic attachments, Canada users can submit an eligibility request.
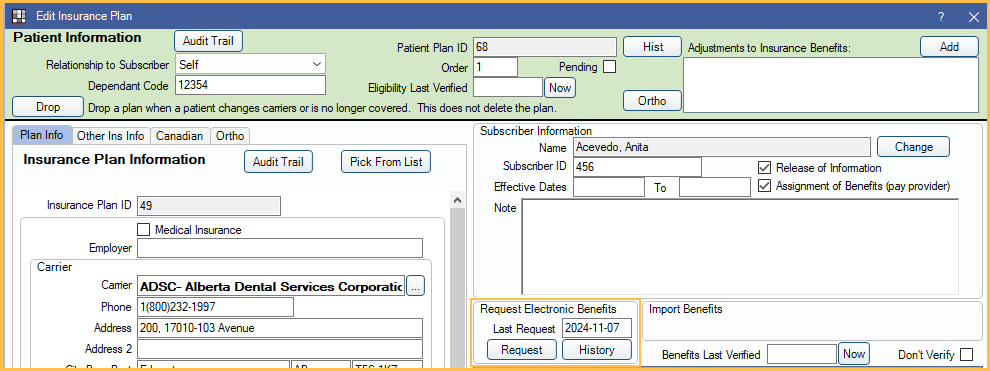
For Canada users, in an insurance plan, use the Request Electronic Benefits section.
Setup
To begin sending electronic eligibility requests, the following must be set up first.
- Set the default eligibility clearinghouse in Clearinghouses.
- Ensure the carrier for the patient supports eligibility.
- Check that the patient's Primary Provider is set to a valid CDA provider in Edit Patient Information.
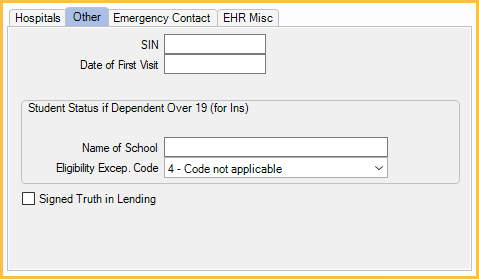
- For the patient, set the Eligibility Excep. Code in the Edit Patient Information: Other Tab. For most patients, use option 4. Cannot be left as option 0.
Eligibility Process
To request eligibility:
- In the insurance plan, click Request.
- A prompt displays showing the eligibility request was sent successfully.
- Close out the prompt.
- Click History.
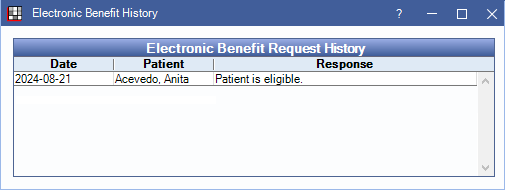
The response displays if the patient is eligible. No additional information (such as benefit details) is available.
